Functional abdominal pain is a common condition that affects many people, yet it is often misunderstood and misdiagnosed. In this article, we will discuss the causes of functional abdominal pain and the various treatment options available to help manage this condition.
What is Functional Abdominal Pain?
Functional abdominal pain is a term used to describe chronic or recurrent pain in the abdomen that does not have an identifiable cause, such as an infection or inflammatory condition. It is a functional disorder, meaning that there is no structural or physiological abnormality that can be detected through standard medical testing.
The pain associated with functional abdominal pain is often described as cramping, burning, aching, or stabbing, and it may be accompanied by other symptoms such as bloating, gas, nausea, or changes in bowel habits. The pain may be constant or intermittent, and it may be triggered or exacerbated by certain foods, stress, or other factors.
Causes of Functional Abdominal Pain
The exact cause of functional abdominal pain is not well understood, but several factors are believed to play a role in its development. These may include:
1. Abnormalities in the way the brain processes pain signals: People with functional abdominal pain may have greater sensitivity to pain signals in the gut, which can lead to the perception of pain even in the absence of any physical damage or irritation.
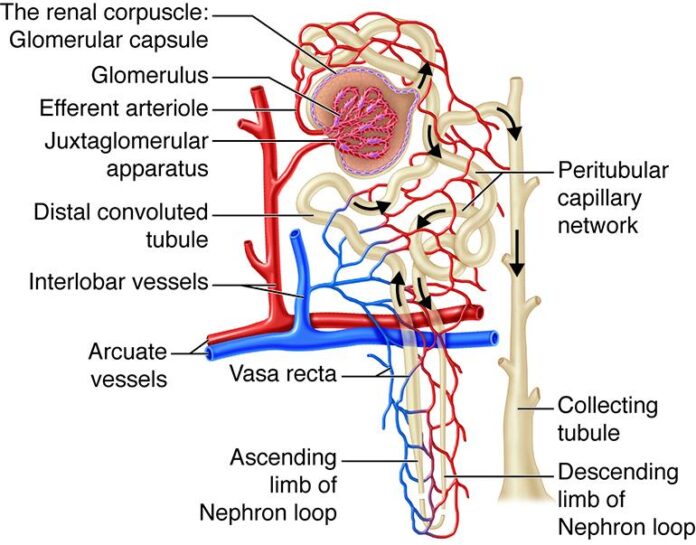
2. Dysfunctional gut-brain axis: The gut and the brain are connected through a complex network of nerves and chemicals that regulate digestion and communicate pain signals. Dysfunction in this system may contribute to the development of functional abdominal pain.
3. Alterations in gut motility: Changes in the way the muscles in the gut contract and relax may lead to abnormal movement of food through the digestive tract, causing pain and discomfort.
4. Psychological factors: Stress, anxiety, depression, and other emotional factors can contribute to the development or exacerbation of functional abdominal pain. These factors may affect the way the brain processes pain signals and the functioning of the gut-brain axis.
Treatment Options for Functional Abdominal Pain
Treatment for functional abdominal pain is aimed at managing symptoms and improving quality of life, as there is no cure for this condition. The following are some of the common treatment options that may be used to help individuals with functional abdominal pain:
1. Dietary modifications: Certain foods and beverages can trigger or exacerbate symptoms of functional abdominal pain. Keeping a food diary can help identify trigger foods, and avoiding these foods may help reduce symptoms. Some people may also benefit from a low-FODMAP diet, which restricts certain types of carbohydrates that can cause digestive symptoms.
2. Stress management: Stress and anxiety can worsen symptoms of functional abdominal pain. Learning stress management techniques such as deep breathing, meditation, yoga, or progressive muscle relaxation may help reduce the severity of symptoms.
3. Medications: Over-the-counter or prescription medications may be used to help manage symptoms of functional abdominal pain. Antispasmodic drugs, pain relievers, and medications that regulate bowel movements may be prescribed by a healthcare provider.
4. Cognitive-behavioral therapy (CBT): CBT is a type of therapy that can help individuals with functional abdominal pain identify and change negative thought patterns and behaviors that may contribute to their symptoms. CBT can also help individuals develop coping strategies to better manage pain and stress.
5. Probiotics: Probiotics are beneficial bacteria that can help regulate the balance of bacteria in the gut. Some research suggests that certain strains of probiotics may help reduce symptoms of functional abdominal pain by promoting healthy digestion and reducing inflammation in the gut.
6. Physical therapy: Pelvic floor physical therapy may be recommended for individuals with functional abdominal pain that is related to abnormalities in the muscles of the pelvic floor. Physical therapy exercises can help improve muscle strength and coordination, reduce pain, and improve bowel and bladder function.
It is important for individuals with functional abdominal pain to work closely with a healthcare provider to develop a personalized treatment plan that addresses their specific needs and symptoms. A multidisciplinary approach that includes healthcare providers from different specialties, such as gastroenterology, psychology, and nutrition, may be beneficial in managing this complex condition.
In conclusion, functional abdominal pain is a common condition that can have a significant impact on quality of life. Understanding the causes of functional abdominal pain and exploring the various treatment options available can help individuals better manage their symptoms and improve their overall well-being. By working with a healthcare provider to develop a personalized treatment plan, individuals with functional abdominal pain can take control of their health and lead a fulfilling and active life.